Healthcare organizations are continually challenged to meet high standards of quality and patient care while also achieving their financial and business objectives. With an eye toward clinical quality measures (CQMs) - many of which health systems are required to report to both payers and regulators - providers are constantly looking for ways to increase efficiency, lower the cost of care, and improve patient outcomes.
That’s where quality improvement (QI) comes in. At its core, QI is a method of continuously examining, tweaking, and re-evaluating processes to make them more efficient and effective. In healthcare settings, QI projects benefit the entire organization and patients by striving for better, faster, safer, and more cost-effective ways of standardizing care.
Using the Model for Improvement in your QI initiatives
The first step in any QI project is to identify a problem that needs to be solved or an improvement that could be made. QI initiatives often stem from CQMs that aren’t being met, for example. Recognition of the problem and a commitment to addressing it gets the project off and running.
Next, it’s time to identify the QI team that will manage the project. The QI team will be tasked with creating hypotheses about the problem and addressing them, including “What are the key drivers of this issue?” and, more specifically as it relates to the electronic health record (EHR) workflow, “What is the impact of alerts, order sets, and orders on the intended outcomes?”
The Institute for Healthcare Improvement (IHI) employs the Model for Improvement as the framework to guide QI projects. The model asks three basic but crucial questions to guide the work:
- What are we trying to accomplish?
- How will we know that a change is an improvement?
- What change can we make that will result in improvement?
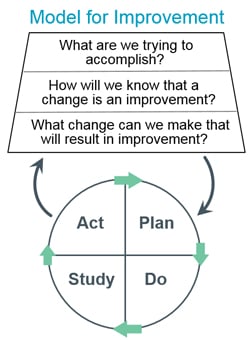
Source: Institute for Healthcare Improvement, How to Improve
Once these questions have been answered, it’s time to put them into action. QI projects should employ an iterative methodology for learning and improvement like the Plan-Do-Study-Act (PDSA) cycle which we described in our recent blog post.
Before digging into an example of a QI initiative using PDSA cycles, it’s important to understand the various players that make up a QI project team.
What are the roles and responsibilities of a QI project team?
Many QI projects have five primary stakeholders who bring complementary experience, subject matter expertise, and sometimes, differing goals and priorities to the table. Here’s an overview of these common roles:
Project sponsor
This is typically an executive or officer of the healthcare organization who has a vested interest in the project. He or she has a direct line to senior management and can help to remove barriers for the team. While not a direct participant in all project meetings, the sponsor will often attend the project kickoff meeting and will review the team’s progress on a regular basis.
Quality Improvement Advisor (or similar role)
A member of the Quality team, often called an Improvement Advisor, serves as the project manager and day-to-day lead for the identified QI initiative. The Improvement Advisor is ultimately responsible for defining the parameters of the project and ensuring it not only gets operationalized, but sustained into practice over time. Additional responsibilities of the Improvement Advisor include:
- Define the project’s goals and milestones. IT and non-technical team members will often have differing views about what needs to be accomplished and how, so it’s imperative that the Improvement Advisor serves as a mediator when it comes to gaining consensus.
- Recruit and select representatives from across disciplines to build the QI project team. These team members will provide input and/or take on tasks related to the project.
- Set up the project kickoff meeting and effectively communicate the identified problem to the team that has been tasked with solving it.
- Set agendas and organize additional meetings, define team roles and responsibilities, create and update necessary documentation and timelines, track deliverables and due dates, and communicate progress, risks, and delays to stakeholders, including the project sponsor.
- Root the project in QI methods by leading the team through the chosen methodology of improvement including the Model for Improvement and/or PDSA cycles, as necessary, which may include more than one iteration to achieve the project’s goals. Once the project is complete, provide an executive summary report or related documentation to close out the project.
Information Technology (IT) team
They’re responsible for implementing the digital and EHR system tools that might benefit clinicians, nurses, and other staff members. IT team members also have the knowledge and expertise to determine what types of systemic changes are possible, the development time needed to make those changes, and what risks or roadblocks the QI project team may encounter along the way.
Hospital staff
A group typically comprised of physicians, nurses, lab technicians, pharmacists, and others - these people bring the necessary subject matter expertise to the QI project. The “eyes on the ground,” patient-facing team members provide a unique perspective that incorporates a human element into the project. They’re focused on not only the end-user perspective of a systemic change (e.g., whether an EHR alert will be effective), but also the patient experience and patient outcomes.
Clinical informaticists
Considered the translators or consultants of the team, clinical informaticists bridge the gap between technical and non-technical teams to help identify the impact of EHR workflow changes (eg. alerts, order sets, and orders) on healthcare quality measures and outcomes. Clinical informaticists will review EHR data - alert overrides for example - and follow through to see how particular events, like interruptive alerts, in the data impacted providers and patients.
Example of a QI project using the PDSA framework
Once a QI initiative has been established, a Quality Improvement Advisor has been designated, and the project team has been formed, it’s time to kick off the project. Using the Model for Improvement and PDSA cycles, here’s an example QI project that’s focused on driving CQMs.
Plan
Let’s say a QI team wants to improve several composite measures related to a sepsis CQM, e.g., assessing initial lactate levels, administering antibiotics, and fluid resuscitation. After assembling a QI project team that includes IT, informatics, three emergency medicine clinicians, and a project sponsor, they collectively decide to build an alert that calls for use of a specific order set (a bundle or “menu” of recommended actions associated with the condition - in this case, Sepsis). Their hypothesis is that this curated order set will make it easier for clinicians to place the correct orders, whether it’s for medications, lab tests, or other orders.
Do
The IT team builds and implements the alert with input from across the QI project team. The QI Improvement Advisor then communicates the implementation to the project sponsor. The QI Improvement Advisor also works with an internal communications leader to ensure the change is communicated across the organization to clinicians, nurses, lab technicians, and any other staff members who will interact with the alert and/or order sets.
Study
The project has been running, the data has been collected, and this is the moment of insight. Did the alert do what it was intended to do? Here’s where the Clinical Informatics team will get involved to review alert data, such as how many times the alert fired, the percentage of overrides, who interacted most with the alert, and whether clinicians used the recommended order set. Alongside the Improvement Advisor, they will look for improved CQMs related to sepsis. The “study” phase of a QI project may take a few days or a few months, depending on the scope of the project and its goals. It’s at this time for project teams that data access, visualization, and analysis becomes paramount, not only for saving effort for the project stakeholders involvement, but to ensure their project moves quickly to an effective outcome.
Act
Based on the findings discovered from the data, the QI project team will recommend a next action. That recommendation may be to maintain the new alert as is, make a change to the alert and/or order set, or iterate on the plan itself and move through the PDSA cycle again.
As you can see, QI is a powerful approach that, when implemented correctly, can help healthcare systems refine and enhance processes that could be more beneficial to patients, staff, or the overall organization. To learn more about the benefits of QI projects, read success stories from Phrase Health clients.
Check out more content
Next: How EHR Alert Data Can Drive Decision-Making in Healthcare

