Overview:
- In the beginning of COVID, a pediatric health system implemented a custom, interruptive alert to encourage N95 usage.
- Fine-tuning the alert triggers to exclude irrelevant providers reduced the alert burden by 50% and may have reduced unnecessary N95 mask consumption.
PROBLEM
There was a lot of uncertainty around viral transmissibility early on in the COVID-19 pandemic. As a result, health systems (along with the general public) were seeking personal protective equipment (PPE) to help face the unknown and limit risk. Public health recommendations identified aerosolizing procedures (e.g. intubations) as particularly high risk and advised N95 use in that setting. With constantly changing recommendations and guidelines, it was imperative for health systems and clinicians to balance being good stewards of limited supplies while also protecting staff.
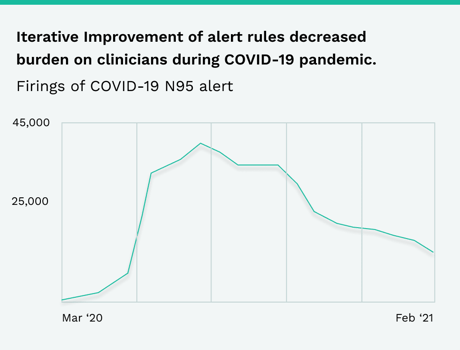
A Phrase Health partner implemented an interruptive electronic health record (EHR) alert in April 2020 that advised health care providers to wear an N95 mask when interacting with possible COVID-19 patients that have an order for an aerosol generating procedure. The alert fired when providers opened a patient chart, so it had a high alert burden (peaking at about 44,000 firings in August). The client’s informatics team initially justified the high alert burden because of the alert’s high acceptance rate (~45%) but eventually turned to Phrase to identify opportunities for optimization.
Open Chart Alerts"The [COVID-19] alert fired when providers opened a patient chart, so it had a high alert burden (peaking at about 44,000 firings in August). The client’s informatics team initially justified the high alert burden because of the alert’s high acceptance rate (~45%) but eventually turned to Phrase to identify opportunities for optimization."
Bombarding end-users with EHR alerts can be counterproductive as inappropriate firings can lead to alert fatigue, clinician frustration, and ultimately ignoring the best practice recommendation. As a result, the pandemic was both an opportunity to educate end-users in light of evolving recommendations, but also a challenge to address workflows that might have been complex even before the pandemic.
APPROACH
The team approached the project with iterative Plan-Do-Study-Act (PDSA) cycles to continuously improve EHR alert performance. PDSA is a quality improvement tool that facilitates assessment and action via an incremental approach. This approach discourages the practice of simply deploying a new intervention (e.g. the COVID-19 EHR alert) and then moving onto the next project without any further adjustment.
From August through November 2020, the team leveraged Phrase Health’s alert analytics to identify providers that did not need to see the alert by looking at groups frequently selecting the “Not going to see the patient in person” response. The EHR alert rules (criteria that define which end-users see the alert) were then adjusted to reduce unnecessary firings and the performance was monitored through Phrase over several months.
Additionally, the team solicited and regularly reviewed clinician feedback through Phrase Health since the alert’s inception in April. The practice of soliciting feedback from end-users is a great way to identify unintended consequences or malfunctions in the intervention build or workflow. Phrase Health lowers the burden
of receiving feedback on EHR interventions by enabling hyperlinks to funnel this feedback directly to appropriate stakeholders. Using this mechanism, several clinicians shared their observations of the EHR alert’s appropriateness within their clinical workflow. This feedback loop allowed the team to identify additional improvement opportunities.
Visualizations made using Phrase Health.
RESULT
The informatics team fine-tuned the EHR alert rules to exclude the irrelevant groups and reduced the alert burden by 50% from August to December 2020 despite the national COVID-19 case rate skyrocketing. Additionally, although the team didn’t explicitly link this EHR alert to their supplies, they believe the change also benefited a related supply chain initiative to decrease unnecessary usage of N95 masks.
The organization’s improvement team continues to regularly monitor this alert’s data. They have also maintained the hyperlink feedback approach. This regular maintenance and monitoring ensures that gains aren’t lost as workflows and practices evolve over time.
PHRASE'S EXPERTISE
Check out more content
Next: Adoption of PDSA Cycles in Healthcare: A Systematic Review
Previous: Beginner’s Guide to Healthcare Quality Improvement